
The Primary Pathways Payment Model is a multi-payer alignment pilot to expand and support pediatric practices in caring for the behavioral health needs of their patients. This pilot is an initiative of the Virginia Task Force on Primary Care, funded by the Virginia General Assembly. The Virginia Center for Health Innovation is piloting the initiative in partnership with Anthem and Sentara Medicaid managed care organizations (MCOs).
Goal: Increase capacity for and quality of behavioral health and primary care for Medicaid children and adolescents.
- Increase training for primary care providers in behavioral health, expanding access to behavioral health services.
- Provide sustainable funding for practices integrating behavioral health into their care.
- Promote increased levels of integration of behavioral health into primary care practices.
- Reduce burnout among primary care providers and behavioral health providers.
- Improve care for children and adolescents with behavioral health needs.
Participating practices will receive two types of payments from participating health plans:
Upfront capacity-building payment to support infrastructure costs
Per member per month (PMPM) payments for all health plan patients based on tier
(payments increase as tier increases)
Practice eligibilty requirements:
- Must be a pediatric primary care practice in Virginia.
- Must be in-network with one or both of the participating Medicaid health plans (Anthem and Sentara Health Plans).
- Applicants should complete VCHI’s Primary Pathways Pilot Interest Form.
Please send your completed Interest Form to zelda@vahealthinnovation.org to begin the application process.
Note: Final selection of practices is determined by the participating health plans.
Participants launching the Primary Pathways pilot include:
33 Practice Sites
202 Primary Care Providers
16 Behavioral Health Providers
16,000 Medicaid Members
BENEFITS FOR PROVIDERS AND PRACTICES:
- Upfront and prospective payments to enable advanced planning for behavioral health integration.
- Support for care management activities that are otherwise not billable services.
- Access to a learning network with other participating practices and resources through the Virginia Primary Care Innovation Hub, such as care compact templates and referral resources.
- A single point of contact at the health plans.
BENEFITS FOR PAYERS:
- Promote whole-person care and early identification of behavioral health needs prior to costly emergency department visits.
- Increase capacity for behavioral health care while supporting primary care providers.
- Promote effective care management of high-needs patients.
- Drive quality improvement through direct incentives for practice change.
- Strengthen relationships with provider networks through direct point of contacts.
- Opportunity for connecting and networking with other participating payers and integrated care providers through monthly meetings and a protected space in the Virginia Primary Care Innovation Hub.
- Leverage market share of other MCOs in addition to your own to drive practice change and promote community partnerships across disciplines.
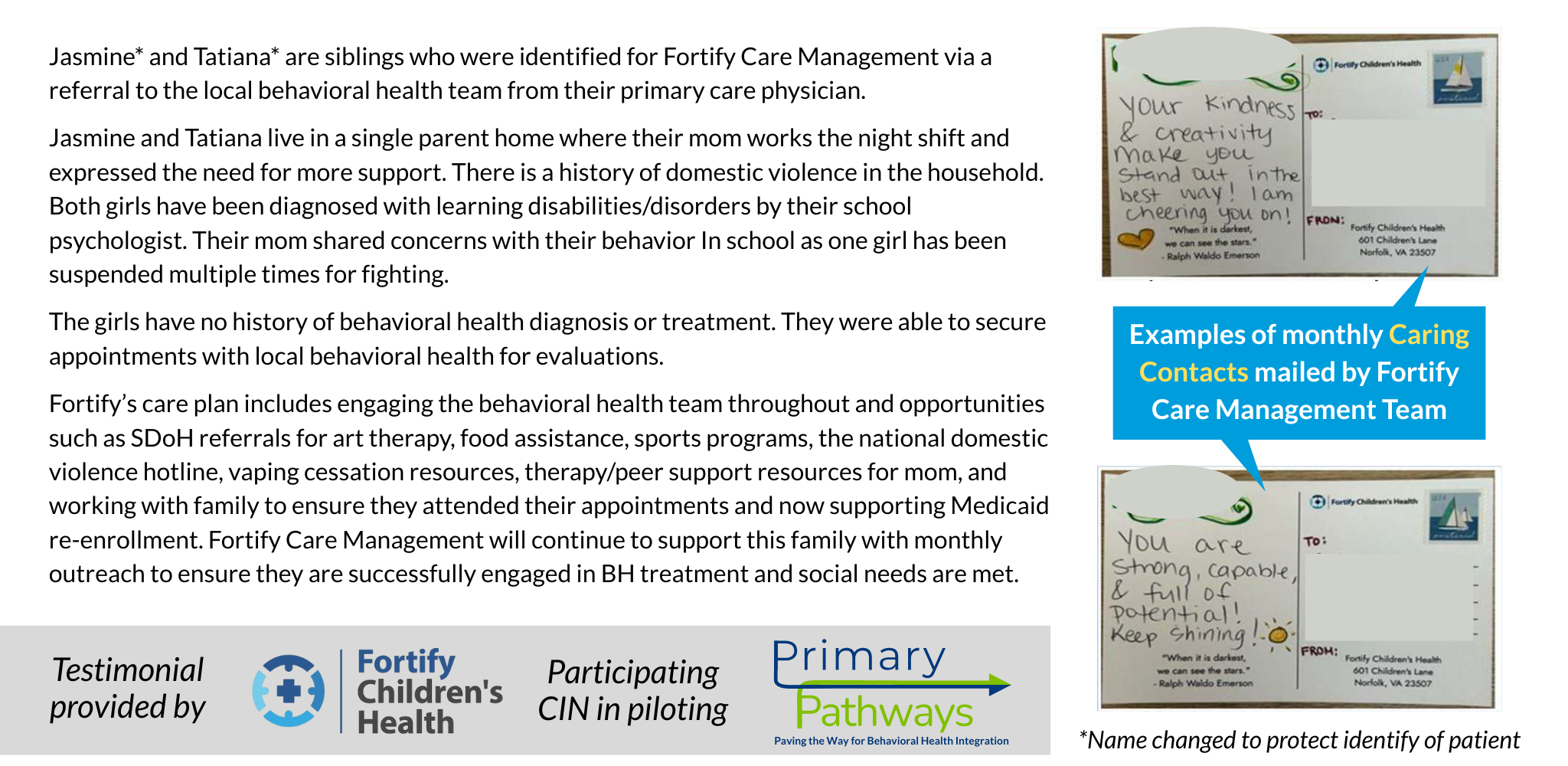
PARTICIPANT TESTIMONIALS:

Previous
Next